UNIVERSITY PARK, Pa. — To repair damaged tissue in the body — from a skin burn to a damaged organ — doctors use collagen, a protein that occurs naturally in tissues. But current methods of using collagen do not use growth factors, which also occur naturally in tissues. These proteins can control how cells function and allow cell growth targeted to a specific part of the body, which in turn would allow for better repair, according to Yong Wang, a professor of biomedical engineering at Pennsylvania State University and the Huck Chair in Cellular Medicine.
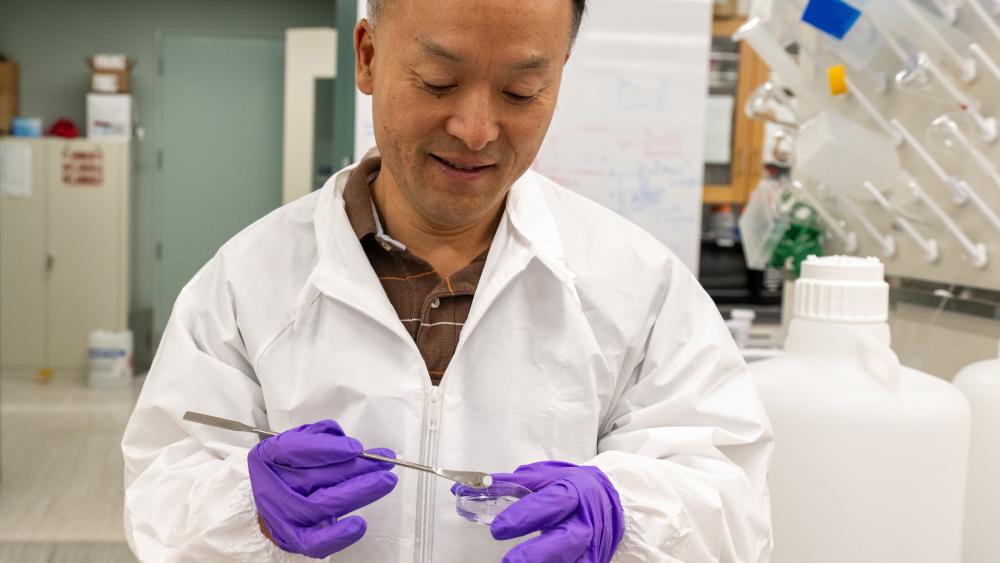
A team of researchers at Pennsylvania State University led by Wang recently received a four-year, $2.02 million grant from the National Institutes of Health to research how to safely add growth factors to the collagen used by doctors for tissue repair.
“Even though collagen alone can help with tissue repair, it is far from optimal,” Wang said. “For example, if we get a burn on our face, the skin will never look the same again, even if the area can recover. This is because if you use collagen alone, a lot of unwanted cells like fibroblasts will grow into the collagen. But if you also use growth factors, they can trigger the growth of the specific cells you want, and then the chance of full facial recovery is much higher.”
Despite these benefits, there is no way to control the rate of growth factor release when collagen surgery is performed. As a result, growth factors are released quickly, making repair less effective and, in more serious cases, leading to rapid cell growth that can lead to cancer.
To solve this problem, Wang and his colleagues plan to use single-stranded, short nucleic acids called aptamers to enable a slow release of the growth factors. This more controlled approach, the researchers say, will likely improve the success of tissue repair without increasing the risk of cancer.
“The main function of aptamers is to bind to the target label,” Wang said. “They can basically bind to anything – viruses, growth factors, cells. In this case, they bind to the growth factors, allowing slow release from the collagen.”
Wang stressed that if successful, her work will have far-reaching implications for the field of surgery.
“When the surgeon performs the surgery – when he cuts the tissue or opens a flap or joins two pieces together or sews them, any kind of surgery – he can use the aptamer to formalize the collagen and thus control the risk of growth factors and thus achieve much better tissue repair or regeneration,” Wang said.
Wang will collaborate on the project with co-investigator Dino Ravnic, an associate professor of surgery at Penn State College of Medicine and the Huck Chair in Regenerative Medicine and Surgical Sciences. Ravnic is also a member of Penn State’s biomedical engineering faculty.